Wistar Scientists Study Ferroptosis to Improve Cancer Treatments
What clues can a cell’s death reveal for immunotherapies for treating cancer and other diseases?
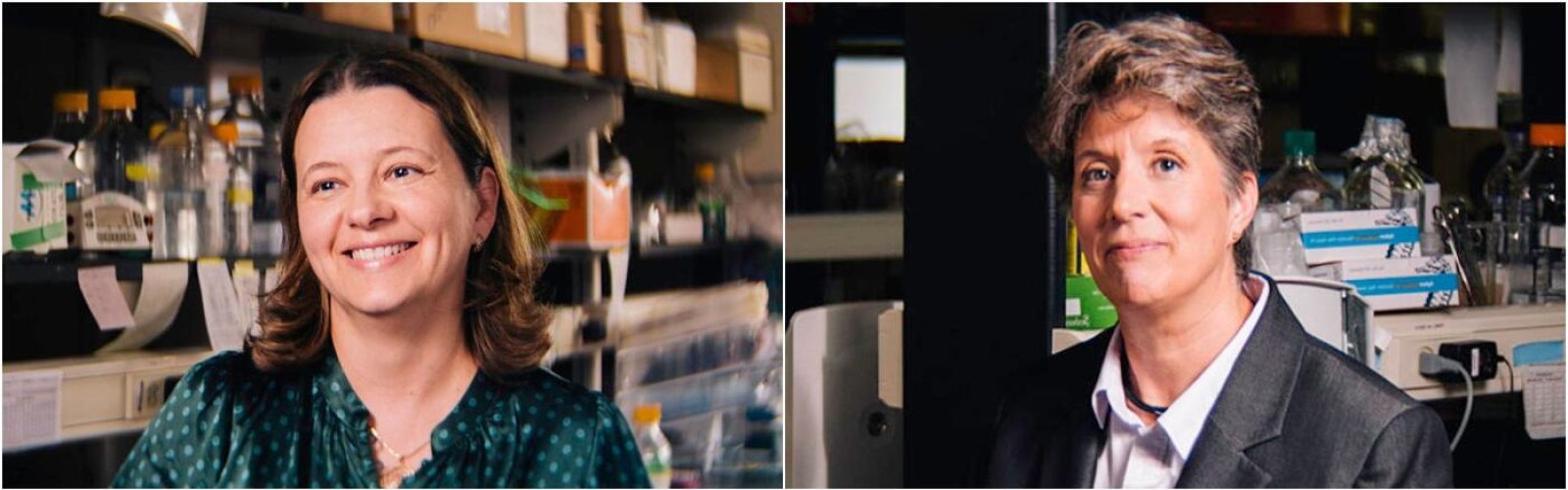
Wistar scientists Dr. Yulia Nefedova, associate professor in the Immunology, Microenvironment & Metastasis Program in the Ellen and Ronald Caplan Cancer Center, and Dr. Maureen Murphy, Ira Brind Professor and program leader of the Molecular & Cellular Oncogenesis Program in the Ellen and Ronald Caplan Cancer Center, are studying a recently identified form of cell death called ferroptosis and how to harness this knowledge to improve care for cancer patients.
Ferroptosis cloaks cancer from the immune system
In a recently published Nature paper, Dr. Nefedova and collaborators reported that ferroptosis occurs in immune cells called neutrophils in the tumor microenvironment. Ferroptosis of neutrophils suppress the immune system and actually aid cancer cells in escaping death. Specifically, neutrophils dying from ferroptosis inhibit one of the most powerful natural enemies cancer has – T cells. T cells are a critical line of defense in the human immune system because they are programmed to attack cancer cells.
“Understanding the mechanisms that mediate immune suppressive activity of neutrophils in the tumor microenvironment is critical to improve the anti-tumor response and efficacy of immunotherapies,” explained Nefedova.
The study demonstrated that systemically or selectively blocking ferroptosis in neutrophils significantly delayed tumor growth and increased host sensitivity to a type of cancer treatment called immune checkpoint inhibitors. Nefedova shared, “Our study identified a new therapeutic approach that could be further explored as a treatment option for cancer patients – especially those who are poorly responding to the existing immunotherapies.”
Ferroptosis could be used to kill cancer cells
“Most cell death pathways occur more in tumor cells than normal cells, so we try to exploit them for cancer therapy,” explained Dr. Murphy regarding her recent paper published in the Journal of Biological Chemistry. Some cancer cells have an increased sensitivity to ferroptosis, and this research uncovered not only why, but how these findings can be translated to improve clinical care of cancer patients.
The Murphy lab studies genetic variants of p53, a critical suppressor of cancer that regulates a protein called PLTP (phospholipid transfer protein). In the study, Murphy and team identified that PLTP can control ferroptosis in cells by controlling the ability of cells to sequester lipids into “lipid droplets”. If a cell isolates toxic lipids into droplets, it can prevent these lipids from penetrating the cell membrane and causing cell death by ferroptosis.
“By identifying lipid droplets as critical for ferroptosis, we identify a whole series of drugs that regulate lipid droplets that can now be exploited to combat cancer,” said Murphy. “We are now exploring the possibility that immune cells use ferroptosis to kill cancer cells. This would help identify people who might be less suited to use immunotherapy to combat their cancers and might have to use extended treatment or a different form of therapy.”