GABRA3 Antagonists for Metastatic Breast Cancer
Unmet Need
Breast cancer is the most common cancer among females worldwide, and it is estimated that approximately 12 percent of women will be diagnosed with breast cancer at some point during their lifetime. While it is considered a manageable disease if diagnosed early, the five-year survival rate for patients with metastatic breast cancer is only 26 percent, and of patients that die of breast cancer, 90 percent die of metastases. No targeted therapy exists for triple negative breast cancer, the most aggressive and metastatic type of breast cancer. The development of therapies that can address the metastatic potential of breast cancer will be crucial to improving the lives of breast cancer patients and their families (1, 2).
Opportunity
We have identified GABAA receptor subunit GABRA3 as a new therapeutic target for metastatic breast cancer. In addition to identifying new small molecule inhibitors of GABRA3, we believe that blood-brain barrier impermeable GABAA antagonists can be repurposed as a breast cancer specific therapy.
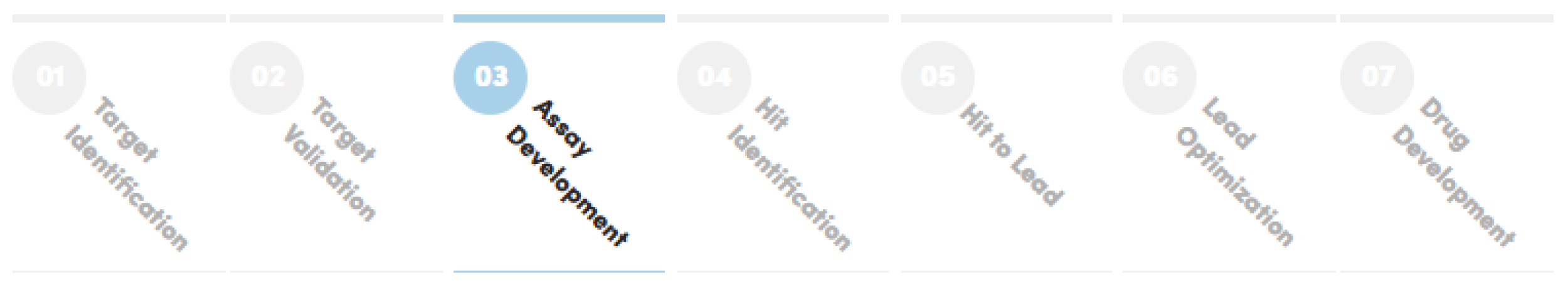
Stage of Development
Analysis of data obtained from The Cancer Genome Atlas shows that higher GABRA3 expression correlates with reduced survival in breast cancer patients. Although GABRA3 is normally exclusively expressed in adult brain tissue, we have recently published that GABRA3 expression is elevated in breast cancer cell lines and tumor biopsies, but not in human mammary epithelial cells. Furthermore, GABRA3 is highly overexpressed in metastatic breast cancers samples compared to primary breast cancer samples suggesting that GABRA3 regulates the migratory and invasive capacity of breast cancer cells.
Noninvasive breast cancer cell lines overexpressing GABRA3 have an approximately 20-fold increase in migration and 30-fold increase in invasion compared to controls, and vice versa, knocking down GABRA3 in invasive breast cancer cell lines results in a five-fold decrease in migration and four-fold decrease in invasion compared to controls. Moreover, 100 percent of mice transplanted with GABRA3-expressing noninvasive breast cancer cells develop metastases, whereas 0 percent develop metastases in the control. Our results suggest that GABRA3 levels and RNA-editing can affect the metastatic potential of breast cancer cells in vitro and in vivo, where higher levels of GABRA3 make breast cancer cells more migratory and invasive, and A-to-I RNA editing of GABRA3 abrogates this effect (3).
Intellectual Property
Our PCT application was filed on January 7, 2017.
Collaboration Opportunity
We are seeking collaborations to (i) identify new NCEs that selectively target GABRA3 subunit, (ii) advance shelved GABAA antagonists that are unable to pass the blood-brain barrier, and (iii) repurpose marketed GABAA antagonists for the treatment of breast cancer and prevention of metastasis.
References
-
Jin X & Mu P. Breast Cancer (Auckl). 2015 Sep 1;9(Suppl 1):23-34.
-
Gumireddy et al. Nat. Comm. 2016 Feb: 7(10715).
-
Brogden RN, & Goa KL. Drugs. 1991 Dec;42(6):1061-89.