Wistar Scientists Explore Importance of Microglia Marker in Metastasized Brain Tumor Microenvironment

-
CONTACT:
-
Darien Sutton
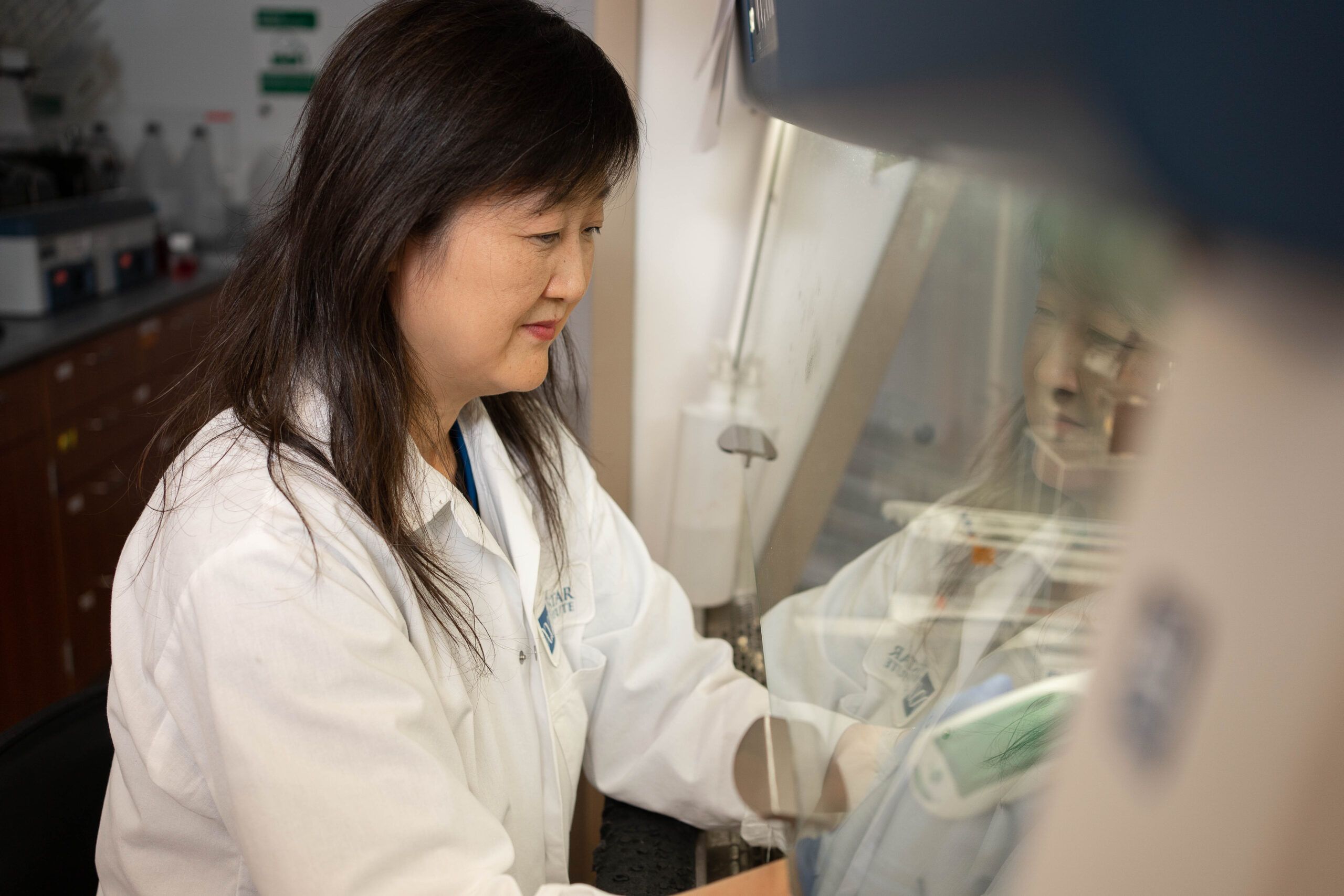
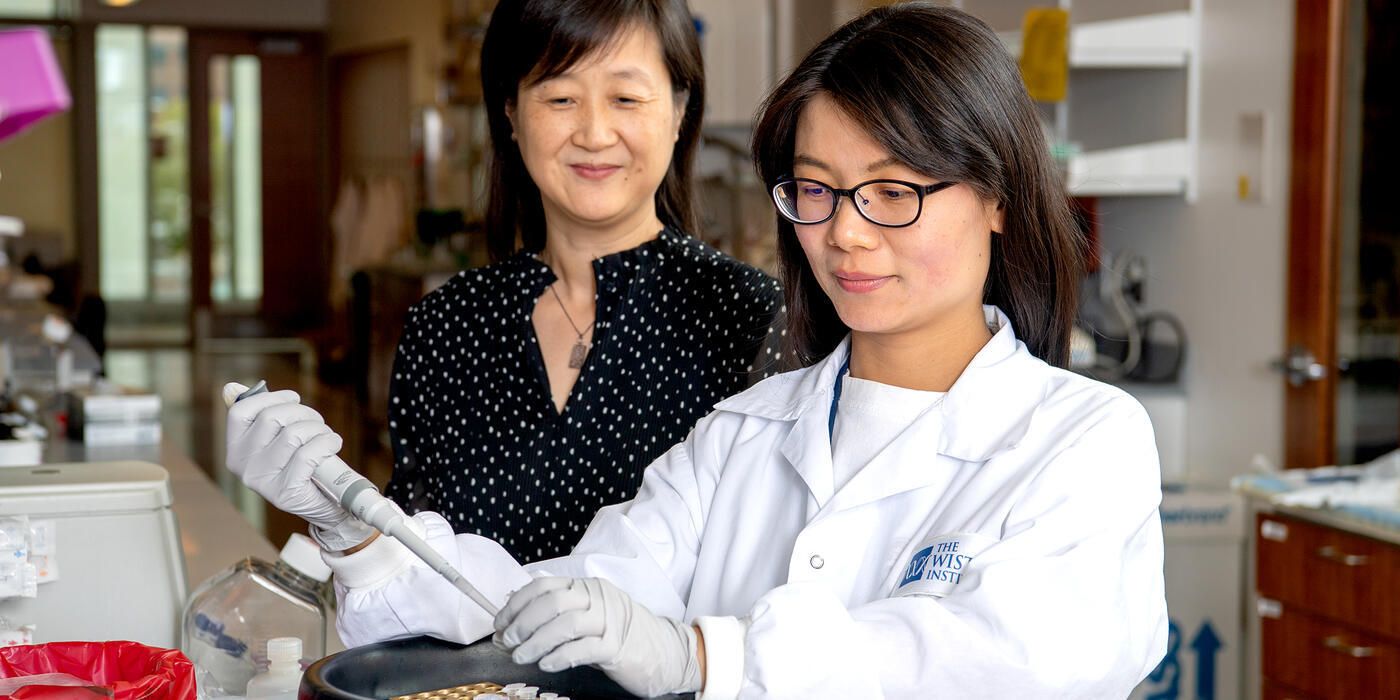
The Chen lab examines microglia activation in metastatic brain tumors
PHILADELPHIA—(Mar. 28, 2024)— The Wistar Institute’s Qing Chen, M.D., Ph.D., assistant professor in the Immunology, Microenvironment and Metastasis Program at the Ellen and Ronald Caplan Cancer Center, has discovered certain immune cells in the brain called microglia have reduced expression of TMEM119 in cases where cancer has metastasized to the brain. The Chen lab’s finding provides an opportunity to more accurately study how brain microglia behave in metastatic contexts, which is key for researching possible therapies. The new paper, “Tmem119 expression is downregulated in a subset of brain metastasis-associated microglia,” was published in the journal BMC Neuroscience.
“This research provides a new avenue and crucial first step in understanding how these immune cells interact with cancer, and we look forward to future mechanistic studies of these cases,” said Dr. Chen.
When cancer cells metastasize into the brain, the nervous system’s immune cells, called microglia, become activated. Immune cells are a very important area of study for cancer researchers because understanding how they do (or do not) function against cancer allows scientists to develop strategies to improve the immune system’s ability to fight cancer.
However, studying the mechanistic role of microglia in metastatic cancers in the brain has been difficult because, by most measures, microglia are difficult to distinguish from another set of immune cells — myeloid-derived immune cells — that also enter the brain in pathological conditions.
Dr. Chen and her lab study how cancer cells interact with brain stromal cells, and wanted to investigate TMEM119 — a cell surface marker which has been recently identified to express specifically on microglia. They aimed to investigate the TMEM119 expression in the microglia from brain metastasis tumors.
They analyzed a preclinical model of breast cancer that metastasizes to the brain, and by assessing the gene expression of the immune cells, her team was able to confirm that only brain microglia, but not infiltrated myeloid cells, express TMEM119. Moreover, metastasis-activated microglia have an identifiable reduction in TMEM119 expression.
Co-authors: Weili Ma, Jack Oswald, Angela Rios Angulo, and Qing Chen of The Wistar Institute.
Work supported by: National Institutes of Health & National Cancer Institute grants T32CA009171, R01CA241490, and Specialized Program of Research Excellence P50 CA261608.
Publication information: “Tmem119 expression is downregulated in a subset of brain metastasis-associated microglia,” from BMC Neuroscience.
For a printer-friendly version of this release, please click here.
ABOUT THE WISTAR INSTITUTE:
The Wistar Institute, the first independent nonprofit biomedical research institute in the United States, marshals the talents of an international team of outstanding scientists through a highly enabled culture of biomedical collaboration and innovation, to solve some of the world’s most challenging and important problems in the field of cancer, immunology, and infectious disease, and produce groundbreaking advances in world health. Consistent with a pioneering legacy of leadership is not-for-profit biomedical research and a track record of life-saving contributions in immunology and cell biology, Wistar scientists pursue novel and courageous research research paths to life science discovery, and to accelerate the impact of early-stage discoveries by shortening the path from bench to bedside. wistar.org