The Wistar Institute Awarded Second National Science Foundation Grant to Expand Award-winning STEM Training Program

-
CONTACT:
-
Darien Sutton
PHILADELPHIA — (May 14, 2024) — The Wistar Institute was awarded a $649,971 grant from the National Science Foundation (NSF) to support the continued expansion of its award-winning Biomedical Technician Training (BTT) Pre-apprenticeship Program. The grant supports Wistar’s reach to community colleges in New Jersey and Delaware who may have limited or no access to hands-on laboratory training and internships. This marks the second NSF grant supporting the Program’s continued expansion.
“As the Greater Philadelphia Region’s life science sector continues to expand, there is greater demand for laboratory technicians in both academic and industry labs,” said Dario Altieri, M.D., president and CEO, director of the Ellen and Ronald Caplan Cancer Center, and the Robert and Penny Fox Distinguished Professor of The Wistar Institute. “This 25-year program has offered career pathways to a candidate pool that is eager to join the life science sector and gain access to both entry-level and long-term careers here in Philadelphia.”
Created in 2000, The Wistar Institute’s BTT Program was initially designed as a two-summer, hands-on, mentored technician training program that prepared community-college students for positions in academic and biomedical, biotechnology, and pharmaceutical laboratories. Originally limited to students from Community College of Philadelphia (CCP), in 2021, Wistar received its first National Science Foundation (NSF) Advanced Technological Education (ATE) grant, Expansion, Curriculum Evolution, and Enhancement during BioTechnician Training (ExCEEd BTT), allowing it to expand from a cohort of 12 students from CCP to a cohort of 20 students from CCP and four other regional community colleges.
The latest grant, Tri-State ExCEEd BTT, will enable Wistar to bring its BTT Program to additional community colleges in New Jersey and Delaware starting in Summer 2025 through Summer 2027. The grant will expand the applicant pool in the Greater Philadelphia Region by including three additional community college collaborators, for a total of eight community colleges covering at least 10 counties in three states for Wistar’s BTT Pre-apprenticeship Program.
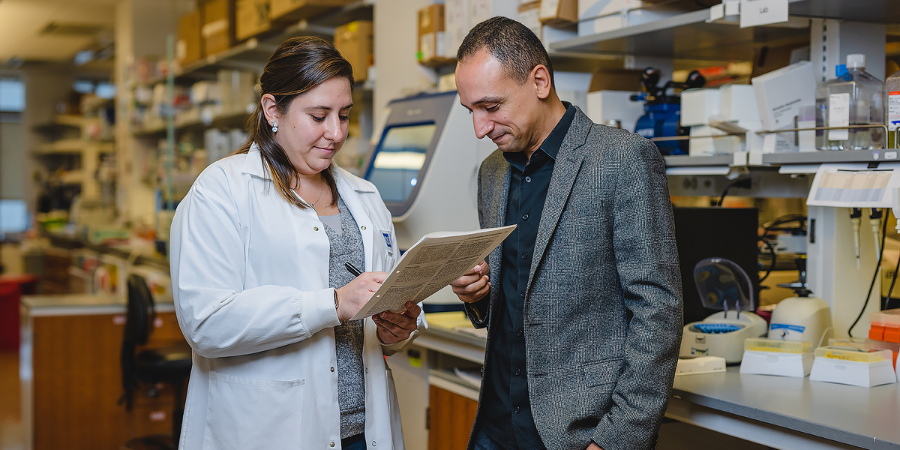
In ExCEEd BTT, students engage in a paid, accelerated, one-summer pre-apprenticeship training that includes a hands-on laboratory orientation at Wistar and two full-time, mentored experiences in academic and industry labs. Program graduates are prepared for immediate employment as laboratory technicians and may also continue training through Wistar’s registered Fox Biomedical Research Technician (BRT) Apprenticeship.
The BTT Program and BRT Apprenticeship provide training and research experiences not typically available to associate degree students, a segment of the workforce that is indispensable to support the success of an ever-expanding life science sector. Tri-State ExCEEd BTT supports Wistar’s commitment to building a diverse and inclusive life science sector talent pool. With this support from the NSF Wistar can expand its programming base and continue to train a diverse and underrepresented student population with limited access to life science research.
“By exposing students to Wistar science, we’re giving them access to the latest research, so they are ideally positioned for future careers,” explained Dr. Kristy Shuda McGuire, Dean of Biomedical Studies at The Wistar Institute. “Our approach is to work closely with faculty at community colleges to develop a cohesive program that offers students the foundational knowledge and the hands-on training they need to be successful. Then they put their knowledge and skills to work with two lab experiences with academic or industry collaborators here in the region doing cutting-edge science.”
Tri-State ExCEEd BTT will also add cell and gene therapy components to the current curriculum, provide a blueprint for incorporating a biotechnician pre-apprenticeship program into various biotechnology and science curricula at community colleges, and serve as a model for regional program expansion. New employer collaborators in two neighboring states will be recruited, allowing the registration of the apprenticeship for use nationally.
For a printer-friendly version of this release, please click here.
ABOUT THE WISTAR INSTITUTE:
The Wistar Institute is the nation’s first independent nonprofit institution devoted exclusively to foundational biomedical research and training. Since 1972, the Institute has held National Cancer Institute (NCI)-designated Cancer Center status. Through a culture and commitment to biomedical collaboration and innovation, Wistar science leads to breakthrough early-stage discoveries and life science sector start-ups. Wistar scientists are dedicated to solving some of the world’s most challenging problems in the field of cancer and immunology, advancing human health through early-stage discovery and training the next generation of biomedical researchers. wistar.org.