PHILADELPHIA — (May 20, 2020) — The Wistar Institute, an international biomedical research leader in cancer, immunology and infectious disease, announces a study reporting initial immunogenicity of a synthetic DNA vaccine for SARS-CoV-2 developed in collaboration with Inovio Pharmaceutical, Inc., and other scientists. Published in Nature Communications, the report focuses on immune studies in animals, which show induction of functional antibody responses and T-cell responses following immunization. The vaccine, INO-4800, was advanced to phase 1 clinical testing in 10 weeks (clinicaltrials.gov NCT04336410).
The SARS-CoV-2 coronavirus emerged in December 2019 in the city of Wuhan, China. Infection causes the viral pneumonia disease COVID-19 that has spread quickly around the world. On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic. Currently in the U.S., there are 1.5 million confirmed infections and more than 90,000 deaths occurring in just months, making COVID-19 infection the leading cause of death in the country.
No vaccines or major therapies are available to prevent infection or control the disease and the U.S. government has made development of a vaccine for COVID-19 a top priority. The viral genome became available on January 11, 2020, and the Wistar-Inovio team immediately began working to design and develop a new vaccine, based largely on their previous experience creating a synthetic DNA vaccine against the related coronavirus that causes Middle East respiratory syndrome (MERS).
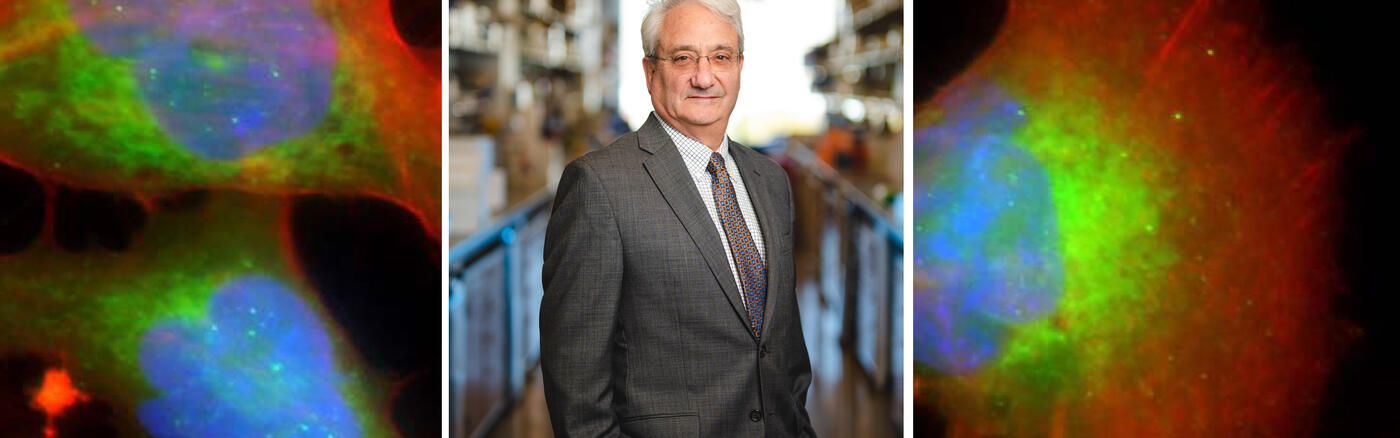
Working with Inovio, a group led by David B. Weiner, Ph.D., Wistar executive vice president, director of the Vaccine & Immunotherapy Center (VIC) and W.W. Smith Charitable Trust Professor in Cancer Research, focused on rapid development of a synthetic DNA-based vaccine targeting the major surface antigen Spike protein (S) of SARS-CoV-2 into preclinical studies.
“We focused on both assay development and vaccination studies to test if immune responses induced by the vaccine in laboratory animals were functional against the virus. Our focus was the induction of immune responses that could in concept make it difficult for SARS-CoV-2 to have a home in the human body,” said Weiner, co-senior author of the publication. “The vaccine was designed leveraging our synthetic DNA technology, which has a set of conceptual advantages including accelerated clinical development built on a conceptually safe, non-live, simple platform that has scalable manufacturing and temperature stability. The vaccine-induced antibodies in vaccinated animals were of sufficient quantity and quality to block interaction of the virus with its receptor, which is its doorway into infecting the body, and were present in the lungs, a place where immunity is very important. The vaccine also induced T-cell function, which is critical for clearing viral infections from the body. These are indications that the immunity it induced might provide no escape for the SARS-CoV-2 virus. We are looking forward to additional studies and examining data from the ongoing clinical trial.”
The team includes Wistar VIC investigators Daniel Kulp, Ph.D., Kar Muthumani, Ph.D., and Ami Patel, Ph.D., who is a shared first author in the paper.
DNA vaccines work by delivering the genetic information required to make a certain viral protein in the recipient’s body, which stimulates the immune system to recognize that protein as foreign and build a response against it, thus targeting the virus and providing protection from infection.
Expressed in vitro, INO-4800 induced robust expression of the S protein. Within days following a single immunization of mice and guinea pigs, the vaccine induced antigen-specific T cell responses and functional antibodies that neutralize the virus, blocking the ability of the SARS-CoV-2 S protein to bind to the angiotensin-converting enzyme 2 (ACE2) host receptor on human cells.
Importantly, SARS-CoV-2-specific antibodies were detected in the lungs of immunized animals, suggesting they might protect against upper and lower respiratory disease that is associated with severe cases of COVID-19.
“While this candidate continues its journey as a potential vaccine against COVID-19, we are continuing our work in the lab to gather more information on the vaccine’s performance in small and larger animals,” said Patel, who is a research assistant professor at Wistar. “We will further characterize antibody functionality, cellular responses, and the ability of INO-4800 to mediate protection of animals against viral challenge.”
Co-authors: Trevor R.F. Smith and Stephanie Ramos from Inovio co-first authors. Other co-authors include Xizhou Zhu, Ebony N. Gary, Susanne N. Walker, Mansi Purwar, Ziyang Xu, Pratik Bhojnagarwala, Neethu Chokkalingam, Elizabeth Parzych, Emma L. Reuschel, Nicholas Tursi, Jihae Choi, Edgar Tello-Ruiz, Mamadou A. Bah, Yuanhan Wu, Daniel Park, Yaya Dia, Ali Raza Ali, Faraz I. Zaidi, Kevin Y. Kim, Sophia Reeder, Makan Khoshnejad, Jacqueline Chu, Kar Muthumani, and Daniel W. Kulp from Wistar; Dustin Elwood, Jian Yan, Katherine Schultheis, Jewell Walters, Maria Yang, Patrick Pezzoli, Arthur Doan, Miguel Vasquez, Igor Maricic, Dinah Amante, Alison Generotti, Timothy A. Herring, Ami Shah Brown, J Joseph Kim, Jean Boyer, Laurent M.P.F. Humeau, and Kate E. Broderick (corresponding author) from Inovio Pharmaceuticals; Nianshuang Wang, Daniel Wrapp, and Jason S McLellan from University of Texas at Austin; and B Wang from Fudan University, China.
Work supported by: Funding from the Coalition for Epidemic Preparedness Innovations (CEPI).
Publication information: Immunogenicity of a DNA vaccine candidate for COVID-19, Nature Communications (2020). Online publication.
###
The Wistar Institute is an international leader in biomedical research with special expertise in cancer research and vaccine development. Founded in 1892 as the first independent nonprofit biomedical research institute in the United States, Wistar has held the prestigious Cancer Center designation from the National Cancer Institute since 1972. The Institute works actively to ensure that research advances move from the laboratory to the clinic as quickly as possible. wistar.org.