Pioneering Biologist Dr. Barbara Knowles Returns to Wistar
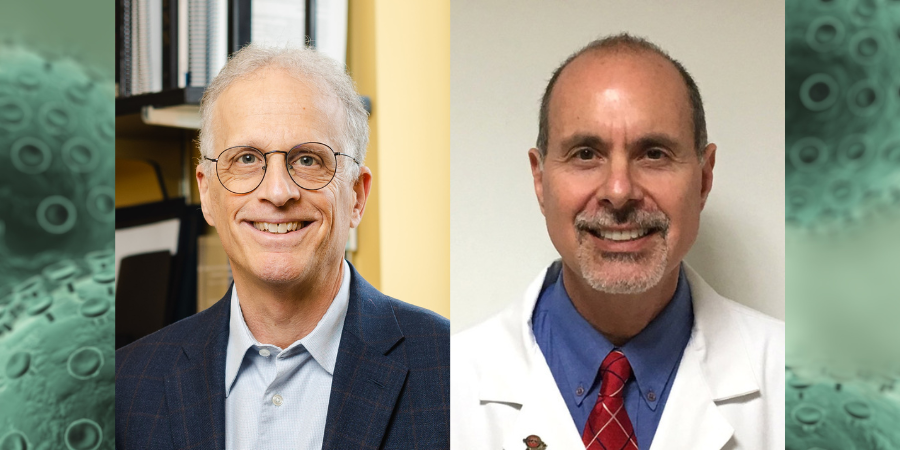
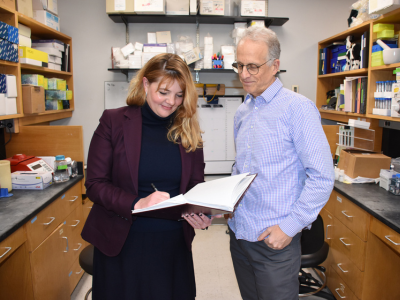
Dr. Barbara B. Knowles’ recent return to The Wistar Institute was timely. The former professor and her family toured Wistar’s newly opened Center for Advanced Therapeutics (CAT). During the visit Dr. Knowles also conferred her blessings on a new $1.5 million endowed professorship carrying her name. The Barbara B. Knowles, Ph.D., Endowed Professorship was made possible by a philanthropic gift from two Wistar Trustees – Sue Dillon, Wistar Board Vice Chair, and Helen Pudlin, former Wistar Board Chair. The permanent endowment supports the recruitment of a cutting-edge, academically excellent research leader to the CAT.
“Barbara’s scientific legacy exemplifies the kind of scientist we want to recruit to Wistar’s Center for Advanced Therapeutics,” said Sue Dillon, “where the unique collaborative environment supports the innovative research needed to solve challenging problems, save lives, and create new and crucial medicines of the future.”
“We are delighted to support this first endowed professorship for the CAT,” said Helen Pudlin. “Named in honor of Barbara Knowles and indicative of her continuous scientific contribution of groundbreaking research, it is more than fitting, and our aim is to bring a new outstanding scientist to the Center.”
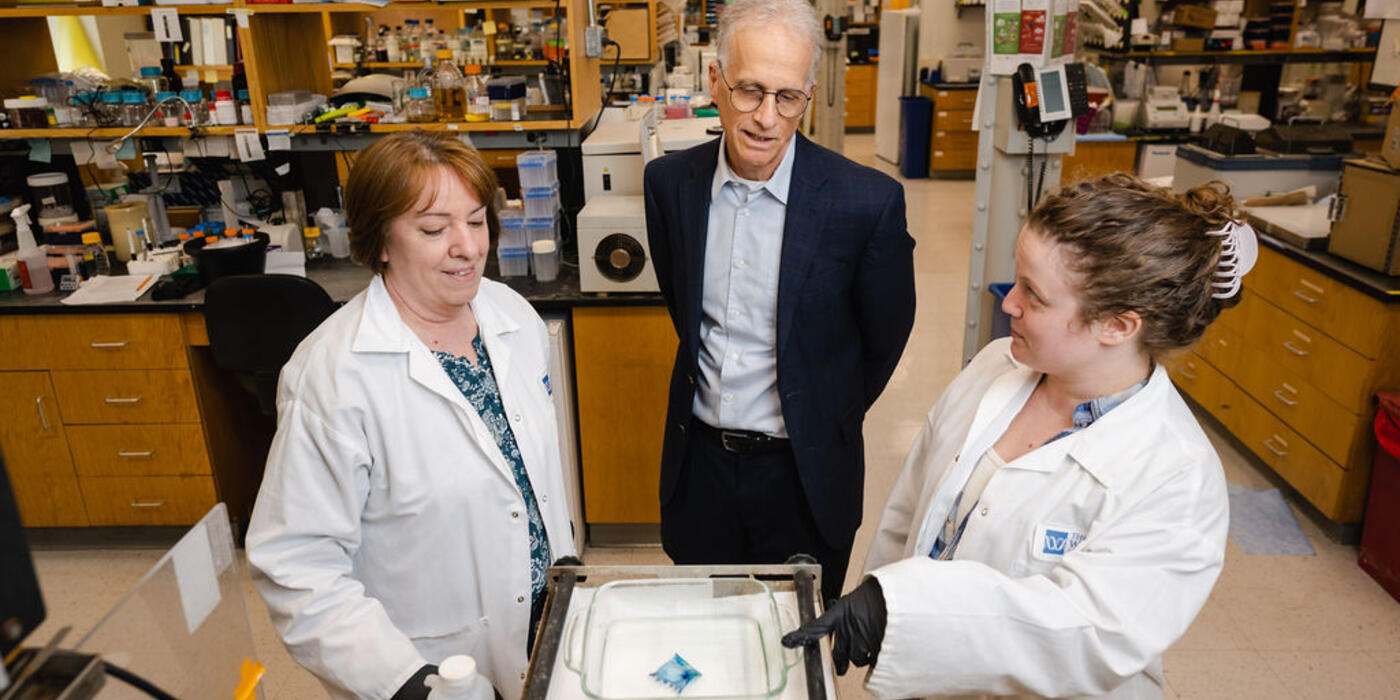
Center director Dr. Paul Lieberman accompanied Dr. Knowles, her husband, fellow retired Wistar professor Dr. Davor Solter, and her two adult children Amanda and Jared Knowles, through the state-of-the-art space built to translate Wistar biomedical research into new future cures.
Seeded by a $30 million philanthropic gift, the CAT will recruit and grow a team to identify clinically attractive assets. Through advanced computational biochemistry, AI, high-tech instrumentation & robotics, Wistar scientists can steward and advance promising discoveries with the end goal of future medicines.
The renown geneticist’s return was a special opportunity to revisit old Wistar haunts and relive the scientific career that established her as a pioneering researcher and major contributor to pluripotent stem cell development. The “HepG2” liver cell line she created is still widely used in biomedical research, biotech and pharmaceutical development around the world. Dr. Knowles also developed important monoclonal antibodies against embryonic stem cell markers that, for the past four decades, have been the critical reagents to identify pluripotent stem cells.
Dr. Knowles was first recruited in the late 1960s by then-director Dr. Hilary Koprowski.
Dr. Knowles did her graduate work and then postdoctoral fellowship at the University of California, Berkeley, working in Drosophila genetics but she did not want to work with fruit flies for the rest of her life. Dr. Koprowski offered her a lab manager position saying, “I could do any scientific research that I wanted to in my spare time”. She says, “I wanted to pivot to study human diseases and for me this was the perfect opportunity in a stimulating environment, which became my scientific home.” Three years later, and pregnant with her first child, Dr. Knowles had developed several therapeutic strategies she wanted to follow but didn’t have enough time to do her own science and also continue running the Koprowski lab. “So, I finished writing up the papers from my thesis and more recent somatic cell hybrid work and just continued writing grant proposals for independent funding at Wistar.”
And she won, in spades.
Surrounded by so many great scientists at Wistar and being an integral part of a dynamic, environment, Barbara collaborated with many researchers at Wistar, including her husband Dr. Davor Solter, and followed her interests in immunology, embryology and cancer to develop cell therapies. She probed the use of somatic cells as a possible enzyme therapy, and explored immunotherapeutic approaches to control SV40 Tumor antigen-induced tumors in pre-clinical models, and then paved the way for developing human pluripotent stem cell therapeutics.
Dr. Knowles went on to become Director of Research at The Jackson Laboratory, Deputy Director of the Jax Cancer Center and founded the Graduate School in Biomedical Sciences at the University of Maine. After retiring from The Jackson Laboratory and the Max Planck Institute for Immunobiology and Epigenetics respectively, Barbara and Dr. Solter were appointed Research Directors in Singapore at A*STAR’s Institute for Molecular Biology, where they finished up and published select aspects of their scientific work, while expanding Biomedical Science in this entrepreneurial Southeast Asian country.
“I became a scientist at Wistar. I had the time to think and interact with wonderful creative people. And that is it.”
And that is everything.