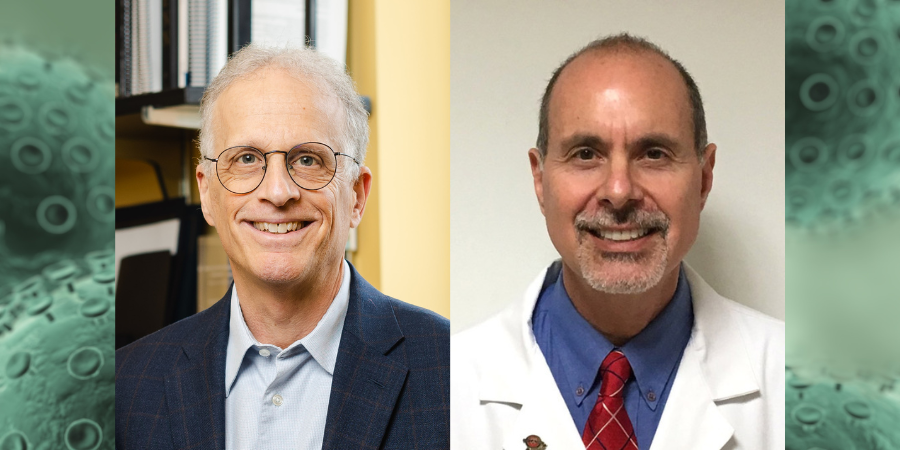
Upon the launch of The Wistar Institute’s new Genome Regulation and Cell Signaling Program, we sat down with the Program’s leader — Hilary Koprowski, M.D., Endowed Professor Paul M. Lieberman, Ph.D. — and co-leader, professor Bin Tian, Ph.D., to learn more about their vision for the Program and what it means for the future of cancer research at Wistar.
Tell us about the importance and excitement in this new Caplan Cancer Center Program.
PL: Wistar has been at the forefront of cancer research and discovery for decades. Recent advances in genomic technology and computational biology have inspired us to establish the new Genome Regulation and Cell Signaling (GRCS) Program. This new Program brings together a team of investigators to solve complicated problems underlying cancer causation, including persistent viral infection, immune response to cancer, and cell signaling changes in cancer.
The GRCS Program combines multi-disciplinary expertise to solve these complicated problems from many different angles: from specialists in genome architecture and integrity like Drs. Tempera, Gardini, and Sarma, who focus on the physical structure of our genome, which has very critical ramifications for genetic diseases & cancers; to investigators interested in virus’ infection and cancer causation, like myself, Dr. Tempera, and Dr. Price; to researchers of inflammatory signals in cancer cells and metastasis with Drs. Chen and Altieri; to specialists in computational and informatic techniques like Drs. Madzo, Kossenkov, and Srivastava, who are essential for effective analysis and interpretation of the vast datasets our Program generates.
How does the combination of genome regulation and cell signaling synergize in this new Program?
BT: We want to better understand cancer, so we study how genes are regulated or dysregulated at the genomic level; cell signaling provides the biological context for understanding how genome regulation plays out in response to internal & external cues. Because of recent technological advances, gene regulation can now be studied across the entire genome — not just individual genes or small groups of genes with similar functions, but all the genes throughout the genome. The synergy between genome regulation and cell signaling is holistic.
PL: Genome regulation does not occur in a vacuum. Metabolic and environmental changes trigger signaling between cells, which, in turn, affect how the genome is regulated. How the genome responds to these types of signals is central to the problems in cancer biology and part of the new focus areas of the GCSR Program.
Why is genomics so critical to cancer research?
BT: All aspects of a cancer cell’s growth — from tumor formation, to tumor survival, to interactions with other cells in the tumor microenvironment — involve rewiring of our cells’ gene expression programs. And that is a fundamentally genome-based process — whether it is a physical change of some genome sequences; alternation of how the genome is structured in 3-dimentional space; transcription of DNA into RNA; or post-transcriptional regulations.
PL: Cancer is a disease of the genome: tumors start when the genome is changed in ways that give cancer a foot in the door. Genomics and informatics analyses allow us to understand the specific genetic changes — which, in cancer, are more like genetic injuries — that drive a particular individual’s cancer. Ideally, once you understand the underlying genetic nature of an individual cancer, you can design precision medicines targeted more accurately to a specific disease diagnosis.
What advances has sequencing technology unlocked in this area of cancer research?
BT: In essence, cancer is a genetic disease. And advanced sequencing technologies have enabled us to examine the genome with the resolution of a single nucleotide — the fundamental building block of DNA. Sequencing technologies have evolved to a point where we can even use these tools to understand the dynamics of genome regulation within individual cells or tiny regions in the body. Essentially, we see cancer’s real-time changes far more clearly, which is key to understanding and combatting the disease.
PL: Advances in genomics and sequencing technologies allow us to understand cancer as a personal disease. Each tumor is different, but we can use precision sequencing as a springboard for researching precision medicine. Armed with the latest advances like next-generation and ultra-high-throughput sequencing — methods that allow scientists to accurately assess entire genomic samples and in minute detail — the new Program’s scientists have the tools they need to move the field even further.
In state-of-the-science Wistar labs, our researchers can easily sample an entire genomic state with tools to improve and expand into new areas of application and translation. Our Program members combine these advances with technologies like CRISPR to identify, target, modify, and correct the genetic aberrations that drive cancer and other genetic diseases.
How do cancer researchers deal with the complexity of the different variables at play in cancer? And how will your Program’s approach account for that interconnectivity?
PL: Due to the complexity of biological systems — and cancer being among the most complicated biological problem because of the rapid, chaotic evolution of tumors and their surroundings — it’s quite unlikely that any single person or brain will solve this challenge. New artificial intelligence applications are welcome tools for investigators; by leveraging AI, we can sort through the massive amounts of biological information and identify potential vulnerabilities within cancer’s framework.
We do work in a reductionist mindset — where the entire complex network of information is reduced to one simple example — to identify new targets and pharmacological agents that can impact the whole system. While that might seem at odds with cancer’s enormous complexity, we still need to simplify the complex science of cancer. It’s a give and take: we zoom in to find a specific mechanism at play in cancer, and then we zoom out to see whether targeting that mechanism can work its way through the vast, interconnected complexity of the disease system to produce a therapeutic effect. We cut through the jungle one molecule at a time.
What is your plan for translating your Program’s discoveries into testable therapy strategies?
BT: We have several promising thematic areas for therapeutic intervention, including the emerging area of gene therapies, as well as continued progress in small molecules as drug candidates. So as we make progress on potential therapeutics, we seek to take full advantage of several technologies and investigate how they work together — similar to the multi-pronged approaches the HIV folks are using for disease containment and cure.
We believe in basic science, which pays off in the long run: any discovery and innovation moves the needle in cancer research and future therapeutics.
Five years from now, what do you hope to have achieved through the Program?
BT: We hope to achieve breakthroughs in both basic science research and cancer therapeutics; we can reach these goals because the GCRS Program has faculty with expertise in many cutting-edge and interdisciplinary technologies and is highly collaborative.
PL: The GRCS program has two main goals: advance our knowledge and understanding of the complex mechanisms of genome regulation and cell signaling in cancer; and second, identify new therapeutic targets and strategies to treat cancer and other complex diseases.
We anticipate publications in high-impact journals to highlight breakthroughs in genome regulation and cell signaling, and we also expect to see some of our findings advanced into new therapeutics — small molecules, gene therapies, and vaccines to treat cancer and other diseases — that will reach clinical trials thanks to our continued collaboration between the public and private sectors.
These are broad and ambitious goals, but they are achievable. With an excellent diversity of scientific expertise and supported by the most advanced technologies available from Wistar’s Shared Resources facilities, the GCRS Program is positioned to find answers to some of the most pressing questions in cancer biology.